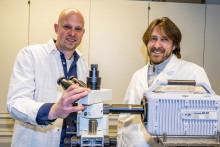
At the University of Twente, the magic often happens at a small scale. This is very true for the research of Guillaume Lajoinie and his colleagues. Lajoinie, assistant professor at the Faculty of Science and Technology, Physics of Fluids, together with assistant professor Tim Segers and Professor Michel Versluis, designed a small chip-like device, shaped like a rectangle, to study the vaporization process of liquid droplets. The device, measuring about one by two centimeters, with two wires attached to one end, turns liquid droplets into gas-filled microbubbles.
Tim Segers carefully puts a thin glass lid on top of the rectangle, creating a small chamber. Then he takes a pipette and inserts a small amount of coated liquid droplets into the chamber. Under the microscope the droplets are clearly visible as tiny transparent balls. Then Segers and Lajoinie attach the two wires to an alternating current. ‘This creates an acoustic wave that drives the droplets into resonance, triggering their vaporization into microbubbles,’ Segers explains. ‘We can follow and film this process through the microscope.’

This new technology happens in less than a microsecond: a slow-motion video reveals that the ultrasound pulse makes the transparent droplets turn dark: the droplets turn into gas-filled bubbles, that have a dark appearance.
Tiny liquid droplets
Microbubbles are tiny gas bubbles, surrounded by a stabilizing shell. They have a wide range of industrial as well as medical applications. For example, they are used in coatings to fireproof buildings, while in medical diagnostics, they are used to visualize blood flow patterns for a better treatment of clogged arteries. However, the medial application of microbubbles has its limitations. Due to their relatively large size, in the micrometer range, they cannot leave the blood vessels, nor penetrate tissue. Therefore, they have limited use for therapeutic purposes outside the blood vessel, for example to deliver medication on site.
‘For diagnostic visualization purposes, microbubbles are perfect’
‘For diagnostic visualization purposes, microbubbles are perfect,’ Lajoinie says. ‘But they are too large to pass through tiny openings in the blood vessel walls, that function as corridors for proteins to move between blood and the tissues.’ Together with his team, Lajoinie, found a solution to this limitation. As a starting point, they used tiny, injectable liquid nano-droplets, that are able to pass the blood vessel wall and enter tissue. Once inside the tissue, the droplets can be vaporized into larger, gas-filled bubbles in a controlled and safe way. This new technology is a start to extend the use of microbubbles to medical therapies, including drug delivery and cancer treatment.

Fundamental science
The transformation of a liquid droplet into a gas-filled bubble requires controlled and safe vaporization of the liquid. This is a complicated physical process that requires a strong focus on the fundamental science involved. ‘Vaporization of liquid requires heat, a reduced pressure, or both. Ultrasound can be an effective way to deliver the energy needed,’ Lajoinie explains. ‘Generating heat to vaporize the liquid droplet, would damage the tissue due to overheating, making it unsuitable for medical applications.’
Therefore, the team came up with another way to vaporize the liquid droplets: by reducing the pressure inside the droplet, vaporization of the liquid can be stimulated. This principle is similar to water that boils more easily at high altitudes, where the air pressure is lower than at sea level.
However, reducing the pressure inside the droplet is difficult and hard to control. Therefore, the team used a new method, where they used low-energy, high-frequency ultrasound. ‘This creates an energy wave, that forces the droplet to resonate: in synchrony with the energy wave, it expands and shrinks very fast. This results in alternating low and high pressures inside the droplet,’ Lajoinie explains. ‘During every ultrasound wave, the droplet accumulates energy. During the periods of low droplet pressure this built-up energy vaporizes the droplet into a gas-filled bubble.’ The beauty of the method is that a reduced ultrasound intensity is sufficient to vaporize the droplet, since it can accumulate the energy needed over time. This makes the process more controllable and is safer for the patient.

Physical destruction
The technology developed is an important step towards the therapeutic use of microbubbles. For example, when treating tumors, droplets could carry medication and once they have moved from the blood vessels into tumor tissue, ultrasound evaporates the liquid, releasing the medication. Another application is the physical destruction of tumor cells. ‘In tumorous tissue, there is a very fast blood vessel growth, resulting in a disorganized blood vessel wall with bigger gaps, around 1 micrometer,’ Lajoinie explains. ‘It is therefore even easier for liquid droplets to enter into the tumor. When these are subsequently vaporized, they physically damage the tumor tissue.’
Important role
Overall, the team has shown that to solve clinical problems, fundamental research has an important role. Although transforming a liquid droplet into a gas-filled bubble could have huge implications for different medical therapies, the method has its limitations. For example, the high frequency ultrasound used doesn’t penetrate very deep into the tissues, and is therefore only suitable for superficial treatment. The application could be extended to deeper tissues by inserting the ultrasound transducer inside the vessels, but this is a more invasive method.
The technology needs some further development to make it fit for use in patients. ‘To apply our basic science of droplet vaporization into a clinical setting, we need to combine our research with applied sciences, where an approved clinical therapy may be developed based on the fundamental understanding of liquid droplets,’ Lajoinie says. ‘We have made an important first step: we improved our understanding of droplet and vaporization behavior with very promising medical applications.’