Since the 1990’s, doctors worldwide have used deep brain stimulation (DBS) to treat movement disorders, including Parkinson's disease and essential tremor, and other conditions such as obsessive-compulsive disorder and epilepsy. During the procedure, surgeons drill holes in the skull and place electrodes deep in the brain. Through a wire under the skin, these electrodes are then connected to a neurostimulator, a device in the patient’s chest which applies electric pulses to modulate brain activity.
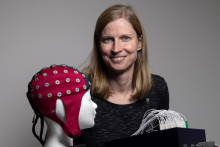
Bettina Schwab
Bettina Schwab is an Assistant Professor in the Biomedical Signals and Systems group, Faculty of Electrical Engineering, Mathematics and Computer Science (EEMCS). Her research generally focuses on systems neuroscience and computational biology, with specific interest in brain stimulation. Broadly speaking, she aims to understand the physiology of the human brain related to motor control. With a background in physics, she investigates the (dys)function of this system using technical methods, including experimental and computational approaches.
More than 200.000 patients accross the globe have undergone this invasive treatment – and yet, nobody knows how and why exactly it works. ‘This has been a big question among scientists and clinicians for over twenty years now, and many people have been trying to figure out the mechanisms of DBS,’ says Bettina Schwab, Assistant Professor in the Biomedical Signals and Systems group. ‘There are many theories, but we are still missing a piece of the puzzle.’ A piece that the UT scientist hopes to fill in. ‘Because there is one factor of DBS that has never been looked at. At all.’ Until now.
'There is one factor of DBS that has never been looked at. At all.’
Schwab’s project DECODE (Desynchronizing weak cortical fields during deep brain stimulation), funded by the ERC, will investigate the influence of this unexplored factor - weak electric fields. ‘The electrodes implanted into the patient’s brain apply electric currents which lead to different electric fields,’ explains the Assistant Professor. ‘Near the stimulation site, the field is very strong, and we can see that neurons directly react to it. However, there are also weaker fields remote from this site, to which the neurons don’t react so clearly. Because of this, they have not been considered important in the outcome of the treatment. I suggest that the weaker electric fields have a characteristically different effect on neural activity, which is harder to capture but might be critical to the success of the treatment.’
Better treatments
At this point, this is only a ‘hunch’, confirms Schwab. ‘I absolutely don’t know if I’m right or wrong because this has never been studied,’ she says. ‘But if the weak electric fields are indeed a critical factor, it could open doors to better treatments. We could use it to achieve better results and less severe side effects.’
This is important because, even though DBS has been an established treatment for over two decades, it’s certainly not without flaws and risks. ‘Our research specifically focuses on Parkinson’s disease. We can see that DBS is often a success for the patients, but it does not work for everyone,’ says Schwab. ‘Some patients don’t have the therapeutic effects we’d like to see, especially when it comes to gait. There can also be serious side effects, such as depression or speech problems. If we’d know where the side effects come from, we could optimize and personalize the treatment. On top of that, we could potentially use the same mechanism for treatment of other diseases.’
Real patients
To explore the mechanisms behind DBS, Schwab and her team will conduct computational modelling to see how the weak electric fields are distributed and how they could be potentially changed. They’ll investigate how neurons react to these fields, focusing on neurons with pathological dynamics such as the ones in patients with Parkinson’s disease. ‘This part of the project is not necessarily risky, because it will allow us to expand our basic knowledge about neural networks,’ says Schwab.
The risky part comes afterwards. When the research findings need to be tested in real life. ‘In the end, we want to know if the weak electric fields are an essential component for the success of DBS – and that needs to be tested in patients who will undergo the procedure,’ says Schwab. For this part of the research, the UT scientist is affiliated with the University Medical Center in Hamburg which implants dozens of DBS devices each year. ‘It will be very exciting to see if the idea holds true. We will be able to gain fundamental knowledge about neurons and neural networks. If we can also apply it and improve the therapy, that would be the most amazing thing.’
'If we can improve the therapy, that would be the most amazing thing’
‘Whether my idea works out or not, I’m super excited about this project. It bridges the gap between fundamental and applied research, between computational modeling and the clinic,’ adds the Assistant Professor. ‘Receiving the ERC grant means a lot to me because it brings an increased independence. I enjoy collaborating with others, but I also want to realize my own ideas and be responsible for the research. If it doesn’t work out, it’s on me. I appreciate that the ERC is willing to take the risk – because this research could be described as an educated shot in the dark.’
ERC Starting Grants
The ERC Starting Grants, provided by the European Research Council, are designed to support early-career researchers who are starting their own independent research team or programme. The success rate of receiving the grant was 14.8% this year. In total, 400 Starting Grants were awarded to young scientists across Europe. Bettina Schwab was the only researcher at the University of Twente to receive the grant in 2023.